
Another application for siRNA gene silencing has been HIV treatment and targeting, which Cell Journal writes about HERE.
Using a humanized mouse model, researchers at Harvard, Seoul and Germany used siRNA to target T-Cells to help combat viral replication of HIV/AIDS, as well as viral infections due to immune-suppression. The first challenge they faced was making a relevant animal model, as they didn’t want to encounter any variants that would be resistant to treatment methods due to the high diversity of sequencing in the virus.
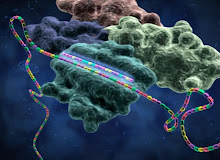
The team used immunodeficient mice that were transplanted with human peripheral blood leukocytes, as well as some transplanted with peripheral blood mononuclear cells from an HIV-1 infected individual (Hu-PBL mice). They overcame the problem of drug-resistant variants by targeting a wide variety of host and viral proteins with siRNA that effectively prevented HIV-1 infection in the mice. The team first looked at the previous success of using antibodies to assist deliverance of siRNA into the cytoplasm of particular targeted cells, which decreases the amount of siRNA needed. They decided to use a CD7-specific single-chain antibody paired with a peptide called 9R. The CD7 antibody was chosen because it is activated by most T-cells and is internalized very rapidly, therefore making it good for siRNA delivery. The 9R peptide was chosen because it had been shown to effectively bind to polyanionic nucleic acids and can be used to deliver siRNA to neuronal cells.
In the Hu-PBL mice, treatment was conducted with a viral co-receptor called anti-CCR5 along with antiviral siRNA bonded to scFvCD7-9R. CCR5 is a chemokine receptor responsible for the fusion between the viral and host cell membranes. With these techniques, siRNA delivery helped control viral replication and prevented CD4 T-cell depletion and even restored it.
These findings help the possibility of new HIV/AIDS therapies by utilizing the receptor-targeting capabilities of siRNA delivery. The team successfully demonstrated that siRNA almost completely blocked viral protein synthesis in HIV-1 infected mice, helped restore T-cell production and suppressed viremia. Nonetheless, in order to integrate this into our current healthcare system, a lot of work still needs to be done.
For instance, delivering large quantities of the siRNA in vivo was very difficult in mice and is expected to be equally difficult in human subjects. Also, new antibodies need to be developed to target macrophages and dendritic cells also infected with HIV-1. Looking at the current pharmaceutical landscape for HIV/AIDS drugs exposes the tough competition siRNA therapy faces in the industry too. With 20 highly effective drugs available, they are administered orally and are much easier to use than the siRNA treatments. They also have years of clinical trials and human efficacy testing to back them.
However, with more clinical research I believe that protein suppression has a lot of potential to treat complex diseases like HIV/AIDS thanks to siRNA’s extremely high versatility. It can target not only the HIV virus, but also suppress acute viral infections that cause respiratory disorders, encephalitis, and hemorrhagic fever—problems that current treatments cannot dually combat. A personalized approach could trigger a paradigm shift in medicine, but costs and procedures need to be reduced and simplified, respectively, in order to integrate into our current healthcare system first.
Another excellent article on this can be found HERE
No comments:
Post a Comment